
FILE PHOTO
Images like this one from the Maryland Republican Party have targeted incumbent Sen. Jim Mathias’ support for safe injection sites. Heroin and opioids have become a focal point of the election.
By Josh Davis, Associate Editor
(Nov. 1, 2018) The heroin and opioid epidemic has touched most communities in Worcester County – and in Maryland.
By all accounts, the face of addiction is the face of your neighbor. They are sons and daughters, mothers and fathers, veterans and star athletes. They are without a single race or religion or class.
You can hear their call in an ambulance siren and, during this election cycle, in the daily reminders of campaign ads from both political parties.
After talking with police and politicians, medical specialists and economists, a mother and father who fought the epidemic by starting a movement, and a former addict who has made it his mission to help others, a common theme emerged: there are no easy solutions.
Nevertheless, plenty of people and resources are being directed toward efforts to save lives and to prevent the tide of addiction from continuing to rise.
Just the Facts
The Maryland Department of Health on Oct. 12 released data for unintentional drug and alcohol-related intoxication deaths from January through June, 2018. During that period, there were 1,325 total unintentional intoxication deaths, a 12 percent increase over the same period in 2017. Of those, 1,185 were opioid-related, including 1,038 fentanyl-related deaths.
According to the health department, more than 75 percent of overdose deaths in 2018 involved fentanyl, a widely used synthetic opioid that’s used both medically and also made illegally and taken as a recreational drug.
Heroin-related deaths decreased 20 percent compared to the same period in 2017 and prescription opioid deaths dropped 7 percent.
However, overall overdose numbers in the state have trended up sharply not only during the last decade, but during the last several years. Unintentional intoxication deaths from January to June totaled 359 in 2008. Since 2012, those have increased each year: 385 (2012); 397 (2013); 528 (2014); 601 (2015); 979 (2016); 1,179 (2017); 1,325 (2018).
Opioid-related overdose deaths numbered 261 in 2008, but shot up to 873 in 2016, up to 1,032 in 2017 and 1,185 in 2018.
There were 13 fentanyl-related deaths during the first half of 2008. The numbers jumped to 469 in 2016, 800 last year and 1,038 during the first six months of this year.
Prescription-related deaths have held more constant: 136 during the first two quarters of 2008, 218 during the same period in 2016 and 199 from January to June of this year.
“Addiction affects families and individuals of all ages and socioeconomic backgrounds,” Maryland Department of Health Secretary Robert R. Neall said in the report. “The Maryland Department of Health, along with our state and local response partners, will continue to improve and expand treatment and prevention options for all Marylanders. If you or someone you know needs assistance, know help is available 24/7 by dialing 211 then press 1.”
Policing an Epidemic: Ocean Pines Police Chief David Massey
David Massey, formerly the police chief in Ocean City, recalled the days when heroin abuse had nearly been eliminated. Now, he said, it couldn’t be more present.
“It’s unlike anything I’ve ever seen as far as addiction,” he said. “There’s no community that’s immune from drug abuse … it’s a national problem and various things have been tried.”
That includes decriminalization efforts, which he said now means “when we get a call for a drug overdose, police can’t make an arrest, no matter what they see.” He said there were unintended consequences to that approach.
“The feeling was that it would make people more apt to call the police,” Massey said. “The unintended consequences are, when we went to a drug overdose before, and we found drugs and someone was arrested, they … would get into counseling and drug awareness, or they would go to a facility. If it was serious enough, they would go to prison and be rehabilitated. Now, we’re not seeing that.”
Today, when police respond to a reported overdose, drugs found at the scene are seized and the overdose victim may be hospitalized, Massey said.
“Or, in many cases, the police [administer] Narcan and just leave,” he said.
Narcan or Naloxone is a drug used to treat overdoses. The widespread availability of Narcan may also be skewing overdose statistics, Massey said. His department was the first in the county to carry the drug and to train police officers to administer it.
Again, there are unintended consequences.
“We don’t have a clue right now as far as how many drug overdoses [are occurring],” he said. “We have the ones that are reported … but we don’t know how big the problem is, because the addicts or the parents of the addicts are keeping Narcan and there’s no requirement to call police [during an overdose].”
Massey said there were 10 fatal heroin-related overdoses in Ocean Pines during the two-year period of 2015 and 2016. Those numbers, which he can measure, have since declined.
“Narcan apparently is working,” he said, adding, “We had one sad case where a woman overdosed 13 times – and the 13th time she died. So, heroin addiction is a very strong addiction. It’s very hard to get off of once it gets a hold of you.
“We have to acknowledge that [Narcan] is bringing people back – the question is, is it a cycle?” Massey continued. “[Does it] bring them back to the point where they can reoffend without treatment?”
Massey said it was his understanding that opioid-related deaths in the United States now outnumbered deaths because of traffic accidents.
“Everyone is looking for a solution – everyone is looking for a magic bullet in the case of opioid addiction, but I don’t think there is one,” he said. “It’s a tragedy and more people are dying from this than anything else in this country.”
He said all ages were affected.
“We see elderly people who were on pills. I’ve seen 61-year-olds … and young people also,” Massey said. “The first time you take heroin you can become addicted – it’s a one-shot poison.”

FILE PHOTO
Kim Poole, a behavioral health and addictions program worker with the Worcester County Health Department, administers a dose of naloxone, a drug that helps reverse opiate overdoses, during a training session at the Ocean Pines Library.
An EMS Perspective: Ocean City Firefighter Paramedics Association President Ryan Whittington
Whittington said the heroin epidemic reached Ocean City about four or five years ago. From there, he said EMS began to see heroin laced with additives such as fentanyl “that were making it much more deadly.”
“In Ocean City and West Ocean City, we see our share of overdoses,” he said. “Heroin is something that is out there. Heroin is an issue that we see not only in Worcester County, but it’s also in Wicomico County … Heroin does not know county lines or state lines. Heroin is everywhere.”
During any emergency call, Whittington said, EMS arrives under the assumption they will be treating someone during their worst day.
“Whether it’s an overdose or a ‘subject fallen,’ our firefighter-paramedics respond knowing that today is someone’s bad day and we have to be there for them,” he said. “When it comes to an overdose call, your situational awareness is always something that’s on high alert.
“You’re looking to make sure that you’re not poked with a needle, you don’t kneel on a needle, that if it is laced with something there’s no residue laying around so that you’d don’t inadvertently touch it … you don’t want it to come through your skin,” Whittington continued. “Your level of awareness is up and you know that, when it comes to an overdose call, seconds matter and you have to be ready to administer your drugs, your oxygen, assist with respiratory efforts – there’s so many things that go on.”
Whittington said Ocean City firefighter-paramedics follow Maryland Medical Protocols, which typically means using Naloxone on overdose victims.
He credited Gov. Larry Hogan’s Heroin and Opioid Emergency Task Force, the interagency coordinating council begun in 2015, with making Naloxone “available to the majority of first responders.”
“That task force has folks from all over the State of Maryland … all these folks together are able to provide things not only for first responders, [but for everyone involved],” Whittington said. “Having those addictions experts, mental health professionals, law enforcement, all of those things have allowed the heroin epidemic to be addressed in the State of Maryland.
“The heroin epidemic is one of the things that I really saw unite all public safety, all communities,” he continued. “I really saw so many people come together from all walks of life to say, ‘We can’t let heroin continue to take over our community – let’s step up and unite and get it out of there,’” he said.
Treating Addiction: Worcester County Health Department Public Information Officer Travis Brown and Behavioral Health Director Christina Purcell
Purcell said anyone seeking treatment is welcome at the health department.
There’s a behavioral health intake and walk-in clinic in Snow Hill open Monday through Friday. On the north end of the county, the health department operates the Worcester Addictions Cooperative Service (WACS) Center on 11827 Ocean Gateway in Ocean City, which treats all manner of substance abuse.
The health department also offers free Naloxone training every second and forth Friday at the Snow Hill Health Department. To preregister, call 410-632-1100.
“We think it’s always good thing that more people have access to this,” Brown said. “It is really a life-saving medication … Even if it’s not an overdose, applying Narcan or Naloxone can’t hurt them, so there’s really no reason not to be trained and to have it, just in case.”
Brown said the health department also emphasizes drug-abuse prevention through several public awareness campaigns, including promoting Good Samaritan laws, trying to reduce the stigma of entering treatment, and the “Decisions Matter” campaign that focuses on connecting people to local resources.
Last spring, the health department began promoting awareness of workplace addiction, especially in the hospitality industry. Brown said of Worcester County Drug Court cases during recent years, “More than 50 percent … have been people who are employed in food service, or hotel-motel.” Last year, more than 90 percent of those cases were related to opioid dependency.
All of the programs are part of a comprehensive effort focused on prevention.
“Just in general, we’ve seen that awareness is growing in the community,” Brown said. “We’ve been focusing a lot on challenges like the preexisting stigma around recovery and treatment, which is something that we are hopefully starting to see the tide turn on … where people are becoming more supportive, more open, more understanding that this is really a ubiquitous problem that affects everyone.
“It’s not any certain demographic … it touches on every aspect of people’s lives in the county, every type of class, every type of age, it’s just everywhere,” he continued. “We do like to remind people that those suffering from addiction who might need to get into recovery – they’re your friends, they’re your family. They’re your neighbors and members of your community, they aren’t just a number.”
Brown said there are additional resources on the health department website, worcesterhealth.org. For access to statewide programs and resources, simply dial 2-1-1.
“If someone needs help, we really just encourage you to support them,” he said. “It can be enough just to have a conversation with someone if you think that they might need help.”
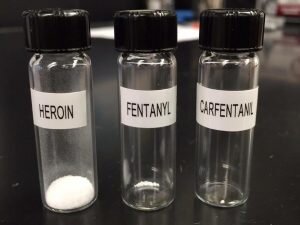
IMAGE COURTESY WORCESTER COUNTY WARRIORS AGAINST OPIATE ADDICTION
The potency of fentanyl and carfentanil, both of which are synthetic opioids, has led to increased overdose deaths statewide, according to the Maryland Department of Health.
In Through the ER: Atlantic General Hospital Vice-President of Patient Care Services Colleen Wareing
Wareing said Atlantic General Hospital staff is attacking addiction and drug abuse on several fronts.
For one, the hospital now uses “care navigators” in the emergency department through a partnership with the health department.
“We are able to utilize their expertise when someone comes in and has any type of addiction – whether it be an overdose, or they may come in for another reason like a cellulitis, but it’s really secondary to needle use,” she said. “That group has been extremely helpful in helping over 200 people since they started back in 2017.
“As a result of their help, as well as other programs, we’re really seeing less of a return to the emergency department,” Wareing said. “In some cases, we can get them into treatment. In some cases, we just plant a seed.”
The hospital has also focused on redefining how its doctors dispense medications that can lead to opiate dependence, including the adoption of CDC standards for safe prescribing and implementing Maryland Hospital Association guidelines for emergency room prescriptions.
“We’re prescribing so few [opioids] in our emergency department now,” Wareing said. “That’s our effort to not contribute to this problem.”
She said membership in the health care company Premier helps to provide benchmarks against thousands of other hospitals, nationally. Additionally, the Prescription Drug Monitoring Program overseen by the Maryland Department of Health requires doctors to review a patient’s history before prescribing some drugs, and AGH pharmacists are now required to prescribe Naloxone along with certain levels of medication.
Many, including Wareing, believe the opioid crisis was born because doctors developed a proclivity to over-prescribe.
“I still believe that is happening, but I think it’s improving,” she said. “I think there’s much more awareness of what these drugs can do and how quickly they can cause addiction than ever existed before. And I truly believe the doctors did not know how quickly people could get addicted to these drugs.”
She said ownership of the problem belonged “in many, many areas.”
“I think the manufacturers of these drugs were really pushing [them],” Wareing said. “We got into a belief system that people should not have pain, which was a very patient-centered model, but then there were also these ‘wonderful drugs’ that the drug companies had that would relieve pain … and it all just snowballs.
“Where did it start – is it the egg or the chicken? I don’t know, but … I don’t believe that anyone maliciously intended for this to get to where it got to. And I think that our physicians are very attuned to the fact that we don’t want to continue to perpetuate that,” she added.
Wareing said the hospital this year is projecting “a decline in actual opioid overdoses.” She acknowledged that could be because of the availability of Naloxone.
“We really are trying to share a lot of data across different things, so the police have data, the Worcester County Health Department has data, we have data,” she said. “Sometimes it’s hard to interpret this data, but it appears that we’re seeing less in the emergency department.”
She added that anyone who has been given Naloxone should still come into the emergency room for treatment.
“Naloxone may reverse it, temporarily, and then the narcotic will take over again and they could end up going back into an overdose situation,” Wareing said. “Not to mention then we could link them, hopefully, to some addictions services – if they’re willing to at least consider it.”
Wareing returned to the issue of where and how the resurgence of heroin and opioid abuse started.
“There’s a whole lot of things that caused the problem,” she said. “It’s a multifaceted, epidemic problem and it’s going to take multifaceted solutions to end it. It didn’t happen overnight and it’s not going to change overnight, but it’s like giving an immunization – if you only immunize 30 percent of the patients you’re not going to control the epidemic.
“With what we’re doing and prevention is doing and Worcester County is doing and the [Worcester County] Warriors are doing and the Atlantic Club, and you put all that together and we keep improving the prescribing methods, reducing the need for narcotics in hospitals, making sure people are educated, making sure people have Naloxone so they don’t die before we can get them help – and on and on and on – it’ll take all of those things until we get to a certain mass and then, without a doubt, we should begin to see this hopefully begin to turn a corner backwards,” she continued.
“I don’t think we know the answer to whether we’re making headway or not, but I do believe 100 percent we’re doing the right things,” Wareing said.
On the Road to Recovery: Hope4Recovery Inc. Executive Director Patrice Ottey
“I can’t imagine there’s somebody out there now that hasn’t seen or heard or had a family member or a friend of the family that hasn’t been affected [by addiction],” Ottey said.
Ottey, also an Ocean Pines Police Detective, has a unique perspective on the heroin and opioid epidemic. Last year she opened a recovery house in Wicomico County. On Monday, she opened the Hope4Recovery house in Berlin.
“I think I’ve learned between two different communities the different aspects of how people respond,” she said. “I see in Wicomico, I think because of the population being a lot bigger, that they respond a little bit differently. It’s very upfront and in your face, and I think people are a little more advanced in their thinking or their accepting [of the problem].
“We hope that having a home here will not just help the guys in the house, but it’ll provide another service to the area and it’ll lessen the stigma,” she added.
As a police officer in Worcester, Ottey often sees people at the peak of their addiction.
“It will be a great opportunity to see them at the height of bouncing back by coming into this home,” she said. “I get to see them starting over, sort of hitting bottom and coming back up, being humble, starting all over, and being thankful. That’s what we’re hoping.”
Hope4Recovery clients are generally admitted after an extended stay in an inpatient facility. Others have been clean for some time, but “need the security of a structured environment,” Ottey said.
All must be drug-tested and have been clean for 30 days. Clients are required to remain drug-free, attend regular counseling sessions, and find employment.
Again, there’s no magic bullet.
“From my experience, there’s not one fix for all – everybody’s journey is a little bit different,” Ottey said. “I will say that the guys that I see that work the steps, go to the meetings and are integrated in that relationship of others in full recovery – they really succeed and they do well.
“I don’t think anybody knows the hard, fast, step 1-25 that’s going to get them where they need to be,” she continued. “But we try to lay the groundwork for what we’ve seen people succeed in. We can only give them the tools.”
By the end, Ottey said clients are hopefully “confident and clean, and a participating member of society.”
“They’re working. They’re giving back. They’re going to their meetings. They’re mentoring … they’re bringing guys up with them and making sure they stay on track,” she said. “That’s one of the huge things we stress at the Salisbury house – you’ve got to pick up a guy that just came in and take them with you, because they’re looking to see what the right thing to do is.
“And happy – I want to see them leave happy,” Ottey continued. “Luckily, the guys that have left to go to independent living have, so far, been successful.”
To contact Ottey about space in the home, email hope4recovery2017@gmail.com or call 443-523-4459.

FILE PHOTO
Worcester County Warriors Against Opiate Addiction co-founder Heidi McNeeley addresses a large crowd during a 2016 meeting
Starting a Movement: Worcester County Warriors Against Opiate Addiction President and co-founder Heidi McNeeley and Fundraising Director Jamie McNeeley
Heidi McNeeley helped start the nonprofit Worcester County Warriors two years ago as a way deal with her own struggle as the mother of a heroin addict.
“Having been down that road as a mom, and knowing how devastating and lonely it was for me, I just felt that it was important to reach out to other people in the community,” she said. “I really just envisioned having a group of maybe five or six family members and we’d meet a couple of times and talk.”
About 50 people attended the group’s first meeting. A month later, the Warriors swelled to several hundred, and now includes local law enforcement and lawmakers, and regional recovery specialists.
“Our mission statement is to educate, support, provide navigation and resources, and awareness to the people of Worcester County that have been impacted by the opioid epidemic,” Heidi said.
Jamie McNeeley said the community’s response has been incredible, especially when asking for donations for fundraisers.
“Nobody says ‘no,’” he said. “In the last fundraiser we had at the Green Turtle in April, we raised close to $5,000 in two-and-a-half hours – and that was mainly from silent auction items that were from community members and business.”
Heidi said money raised “helps people overcome financial obstacles to recovery.”
Half of the funds raised during the Third Annual Rock for Recovery event, Nov. 11 at Trader Lee’s in Ocean City, will go toward the Hope4Recovery house in Berlin.
Recovery homes aren’t free, Heidi said, and often require security deposits and weekly fees.
“A lot of the requests are for the first two weeks in a recovery home,” she said. “We’re going to help fund the first Berlin resident [at Hope4Recovery] and we’re very excited about that.”
The Warriors have also paid for taxis to treatment facilities in Baltimore and for storage units for people entering recovery. Heidi said the group has helped 52 people receive treatment.
“I think what we’ve learned specifically about helping people is to let all the qualifiers go by the wayside,” she said. “Initially, we said we don’t want anybody with a criminal record, because we didn’t want to help them go out of the county or out of state. We only wanted to help people who were Worcester County residents. We didn’t know about helping people a second time, if they relapsed.
“But, we want to save lives, so who really gives a shit if they’re from Somerset County?” Heidi continued. “We’re still cautious, but I think we just want to help everybody that we can.”
She also changed her opinion on supporting harm-reduction tactics.
“When we first started the Warriors, I would’ve been completely against needle exchanges and safe-injection sites, and now I’m 100 percent for them … because it’s something that could save someone’s life,” Heidi said.
“Having been around people who are seriously addicted on a weekly and a daily basis … what I’ve learned is that these people are beautiful, wonderful, dear, sensitive, incredible people,” she continued. “Just because somebody is addicted to heroin, I don’t want to feel like it’s OK for them to die.”
Heidi said there’s no formula for when and how a drug addict will ask for help. The point is to keep them alive until that moment comes.
“If that magic moment occurs and they say, ‘I’m ready for recovery’ and I happen to be there, I can say, ‘awesome, let’s get you on the path,’” she said.
She also understands there is no stereotypical addict.
“An addict looks like a 9-to-5 businessman in a button-up shirt and tie. An addict looks like the high school football star or the MVP of the wrestling team,” she said. “I think an addict looks like any one of us and many of them come from good, loving families.”
A Former Addict’s Take: Tom Mcgrath
Mcgrath is a former resident at Ottey’s recovery house in Wicomico County. He’s 29, originally from Baltimore, and a graduate of Stephen Decatur High School.
He and said he was a normal kid growing up, although he never knew his mother and was instead raised by his father and two brothers.
In college, Mcgrath transferred from Wor-Wic to the University of South Carolina, but a loan fell through during his second semester there. He left school and enlisted in the U.S. Navy.
He smoked marijuana and drank a little, but didn’t try any hard drugs until he came back from the Navy and found his friends had gotten into Percocet.
“Just one day, randomly, I was over at a guy’s house and he was prescribed them,” he said. “I guess I didn’t really open my eyes enough to see how it was grabbing people and catching people, because even my friends at the time were doing it every day.”
It also grabbed him. Mcgrath found the pills helped numb everything that had been going on inside him.
“I wish I would have focused more on things that were going on inside of me, as far as depression and anxiety and just turmoil constantly,” he said. “My head was constantly just going, going, going. I didn’t know how to fix it, so I did drugs.”
He graduated to heroin a few years later when the supply of prescription opioids became scarce. Mcgrath, who sold pot in college, found himself selling heroin to support his new habit.
“I was just trying not to pay $500 out of my pocket,” he said. “I could sell some and still get high. It was like an avalanche … it was probably the most powerless and vulnerable I’ve ever been.
“Once it gets ahold of you, that’s when the real terror starts to come, because it’s not just about the physical addiction anymore … but now it’s in your head,” Mcgrath continued. “Everything snowballed so fast.”
He got busted and charged with distribution, and eventually went to jail. While there, Mcgrath said, the problem only grew worse.
“It kind of multiplied the problem, because then you put me around other people who are addicts and have different connections, and you’re surrounded by that 24-7,” he said. “Once I got released on parole, I went right back to using.”
Within the space of just a few years, two of his best friends overdosed and died. Before that, his aunt had overdosed and died in 2012 and a cousin suffered a fatal overdose in 2009.
“I was still using at that point [around 2016],” Mcgrath said. Finally, he checked himself into rehab, but by doing so violated parole and was again sent to jail.
“The day before I got released, my other best friend left to go back to work on a tugboat in Philadelphia. Two weeks later, he overdosed on the boat and he died,” Mcgrath said. “It was a point in my life where I was saying, ‘Am I going to go left or right?’”
The drugs, he said, had become a mask for unresolved issues with his family and friends.
“I told myself I was either going to be a 50-year-old junkie, or I’m going to try and take a second chance at life,” Mcgrath said. “And it was the first time in my life I felt like I got outside of myself – it wasn’t all about me anymore. I could see the pain in my father’s eyes and my brothers’ eyes.
“I couldn’t do it by myself,” he continued. “And [recovery has] been the greatest thing that’s happened to me in my life, because now, in return, I can help other people that were in that position.”
He got into the drug court program, which he’s now nearly finished, and volunteered to help in several other local groups, including the Worcester County Warriors, that address addiction, depression and anxiety.
“Anything where I can get some personal time, because that’s what I needed,” Mcgrath said. “I needed somebody to get through to me, to pay attention [and to say] ‘I’ve been through it.’ You can have a piece of paper that says, ‘I can help you,’ but you have no idea what I’m talking about, because it’s hell.”
Mcgrath said trying to help someone recover from an addiction is a balancing act. Based on his experience, too much pressure can push someone away, while not enough can make a person feel isolated.
“It’s really individual,” he said. “Really, it’s up to you as far as, ‘Am I tired of this life 100 percent?’ And it can’t be 99, because at 99 percent you’re going to use again. It has to be 100 percent and you have to stay committed.
“You can’t ever stop working, even if it feels like it’s getting better and you’ve been clean for a while … you still have to work every day to replant the different seeds in your head,” Mcgrath continued. “And it’s impossible to do it on your own.”

FILE PHOTO
Del. Mary Beth Carozza speaks during a Worcester County Warriors Against Opiate Addiction meeting.
Prosecuting the Problem: Worcester County State’s Attorney Elect Kris Heiser
Heiser called for a more proactive approach toward the opioid epidemic, and one that transcends traditional roles.
“If I prosecute the case and I win and justice is served and the bad guy goes to jail … can I go home and sleep at night? Yeah, I can go home and sleep at night. I’ve done my job, technically speaking,” she said. “But, if I’m just banging my head against the wall and we’re not getting to the underlying issue and all of the resources are available for me to access and I know the person that needs the help, common sense would dictate that you do a bit more.”
There are difficulties in coordination, however, and she underscored the fact that there’s no one person to call when battling heroin and opioids in the state. So, those involved often have to get creative.
“I’ve spoken with Diakonia, I’ve spoken with Worcester Youth and Family, I’ve spoken with Worcester Warriors Against Opiate Addiction … and they kind of agree that there’s not really somebody divvying up the resources appropriate and making sure everything is covered,” she said. “That’s a big part of it.”
At the other end, Heiser said, is arresting drug dealers who are “pushing the poison.” But that can also be tricky.
“There’s always another one to topple,” she said, adding in 2016 close to 90 percent of Worcester overdoses “were linked to sources not in Worcester County – they were linked to Sussex County.”
“We have a multijurisdictional problem, because Worcester County and Sussex County … don’t have a memorandum of understanding as far as that goes,” Heiser said. “So, now we’re talking about contacting the governor’s office and getting Gov. Hogan to contact Delaware’s governor to make sure Delaware’s problem isn’t bleeding into Maryland in a way that we can’t manage.”
“Identifying the problem is a problem,” she added.
There’s also the matter of a potentially massive lawsuit Heiser compared to the 1998 “Tobacco Master Settlement Agreement,” when 46 states sought to recoup health care costs by suing several of the largest tobacco companies. The settlement in that case included, among other stipulations, more than $200 billion in payments.
Heiser said pharmaceutical companies were “100 percent” responsible for spreading the opioid epidemic, but “the problem there is how to hold them accountable.”
“The fact that the drug manufacturer is pretty much the full basis of information for the doctor is kind of scary,” she said. “When you explain that to people they’re like, ‘well, that doesn’t really make sense.’ These people that stand to make a profit are the only ones that are really advising doctors how much to prescribe and when? That seems a little bit crazy.”
Washington, D.C. based Principal Law Group is handling the case, Heiser said, and she was told the payout to local governments could amount to a decade’s worth of police budgets.
“When they have forensic accountants that are telling us 86 percent of people who overdose on heroin started out by using [prescription] opioids and, therefore, 86 percent of costs of that the government spends to try and contain this problem can be linked back to the pharmaceutical companies and distributors? That’s huge,” she said. “I don’t think it can be overstated.
“I have just been trying to raise awareness that it exists, it’s out there, and I don’t want Worcester County … to potentially miss out on something that could be so helpful for all of our citizens,” Heiser added.
Assessing the Economics: Dr. Memo Diriker, director of the Business Economic and Community Outreach Network of the Franklin P. Perdue School of Business at Salisbury University
During the next several years, Diriker claims, the negative economic impact of heroin and opioids will exceed the positive impact of the billion-dollar poultry industry.
“We did a study on the economic cost of substance abuse in our nine [Eastern Shore] counties,” he said, adding that incarceration, treatments and even the prices for Naloxone were on the rise. “Separately, we did a study of the economic value of all resource-based industries in all of Maryland’s counties. From that, we looked at the positive economic impact of poultry within those resource-based industries.”
The negative dollar-amounts in dealing with the opioid crisis were alarmingly close to the positive impact of poultry, Diriker concluded.
“I don’t remember the number off the top of my head, but they were very close to each other,” he said. “Given that the impact of opioids continues to grow at a very rapid clip, we believe that within in a few years the negative impact will be a higher number than the positive number for the poultries.
“Obviously they’re not related, but the numbers are scary,” Diriker added.
So, what do you do with that data?
“Nothing, other than you make sure that more counties are doing what Wicomico County is doing, because Wicomico County is one of the few counties that has actually reduced the overdose deaths,” he said.
For instance, Diriker said, Wicomico staffed a call center with former addicts to help those in crisis.
“They are encouraged to seek treatment. It’s a nonincarceration, more treatment-oriented intervention service that is delivered primarily by former addicts who have managed to get out of it,” he said. “Unless we do things like that to reduce overdoses and overdose deaths, we’re going to be in even more dire straits than we are [now].”
Overall, Diriker said, in the nine counties he studied, overdoses were increasing – when he factored in fentanyl.
What’s more, he said, the problem was found statistically to be ecumenical.
“All kinds of ethnic and economic backgrounds, all kind of demographic backgrounds [were represented]. You’d never guess who the next person is,” he said. “It’s something we’d better tackle, otherwise it’s going to be keep costing us more and more.”

FILE PHOTO
Sen. Jim Mathias speaks with Worcester County Warriors Against Opiate Addiction co-founder Heidi McNeeley prior to a public event.
Campaigning for a Solution: District 38 Sen. Jim Mathias and District 38C Del. Mary Beth Carozza
The race for Maryland’s District 38 Senate seat has seen both parties trade barbs over policy. Not the least of which was an ad by the Republican Party that suggested Mathias’ support for supervised safe injection sites amounted to the incumbent “making it easier to get heroin than ice cream.”
Carozza said she “took such a strong position against the bill that would allow for heroin-injected sites paid for by the taxpayers,” because it did not have local support during meetings she attended.
“Not one person advocated or supported that approach,” Carozza said. “While I understand that the incumbent is making the point that everything should be on the table with the epidemic this severe, I disagree with that approach, because I believe the initiatives that we move forward should reflect local support and local consensus. So, I strongly oppose that bill and will continue to do so.”
Instead, she advocates allowing for “a very narrowly drawn privacy exemption” to notify parents of college students in cases where drug abuse is suspected. Carozza said the idea came from a series of community meetings that included the Worcester County Opioid Intervention Team.
“I would not move forward on that initiative unless it had local support, so we took this idea that came from this community event with the families of the addicted, took it to the next OIT meeting in Worcester County … where the general consensus was that there would be support for moving forward,” she said. “I plan to continue to do my research and to introduce a very narrow bill to allow for that notification, because in the end I believe that could save lives.”
She said her approach is both comprehensive and “always ties back to the local level.” Carozza also supports increased penalties “for those distributors who are making their money off of the heroin/opioid epidemic.”
“I recognize that, along with recovery and treatment, you have to support this piece of it as well,” she said.
She credited Hogan for being the first governor to declare a state of emergency because of heroin and opioids, and for appointing former Ocean City official Clay Stamp to the statewide task force.
“I plan to continue to be a leader in working with the locals and advocating at the state level so, in the end, whatever programs and solutions we move forward with truly benefit our local families of the addicted and saving more lives, and I believe we can do so with this local approach.”
Mathias likewise praised Hogan’s campaign against opiates, but said the problem is getting worse despite those efforts. He pointed to the state statistics that show the significant annual increase in opioid intoxication deaths.
He went on to say it’s the job of the legislature to consider any “tools that are proven to be effective – regardless of what that tool is,” and shrugged off negative campaign mailers as shock value.
“In this case, that tool was a clean injection site, which was under the auspice of the Maryland Health Department … and a participating local health department opting in,” Mathias said. “We never got to the final lines of this, because of all the furor that was raised.
“We’re trying to bring some responsible compassion and some understanding, but it brought the whole stigma back to rest on the families of those who are fighting this addiction issue and those that are in recovery,” he said.
Mathias compared the legislature to a workbench where elected officials seek to solve common problems. On the heroin epidemic, he said the statistics show “it’s clear that what we have done is not enough.”
“It’s wholly unacceptable that we have to default to what the traditional means can be, and the traditional means have to fall first before we can start looking at things that are working in other places that are creative,” Mathias said. “I was able to make that change in cancer [research]. I’m willing to discuss making that change in addiction.”
“I’m going to continue to not wait until something fails first,” he continued. “With the increases in the death rate, it’s clear that we don’t have the full measure that we need and all the toolboxes that we need to effectively address addiction and mental health … and I’m going to stand up to make sure that we get those.
“I am not going to stigmatize or stymie a creative thought for conversation at the workbench of Maryland,” Mathias said.
